Ten years ago, the world
was in the grip of a panic over an outbreak of a mysterious illness -
Sars. The virus killed hundreds - and infected thousands more - but its
impact would have been far more devastating had it not been for the
bravery of a handful of doctors and nurses.
"It was like a nightmare - each morning you arrived and more people were sick."
In 2003, Dr Olivier Cattin was working at the French hospital in Hanoi, in the north of Vietnam.
"We got to the Friday and there was only one nurse left on
our ward who was able to treat the other nurses, and this nurse was also
sick."
One day at the end of February that year, a Chinese-American
man, Johnny Chen, had arrived with what appeared to be a bad case of
flu.
Within days, nearly 40 people at the hospital had fallen ill,
including a number of the staff. Seven would go on to die. This was the
site where the deadly disease - later named severe acute respiratory
syndrome (Sars) - would come to the attention of the world.
It was highly contagious, and often deadly. More than 8,000 people around the world were infected, and more than 770 died.
Continue reading the main story
Find out more
Kevin Fong was reporting for a two-part
BBC World Service documentary
Sacrifice: The Story of Sars.
Part 2 airs on Sunday at 14:06 GMT (15:06 UK time)
But this is a story about people
not statistics. The closer you get to the story of Sars, the more
overwhelmed you become by the experience, and the heroism, of those who
stood on the frontline.
War is a metaphor that we often use in relation to the fight
against disease. But it is rarely more apt than in the case of Sars.
At the French hospital in Hanoi, panic set in as the doctors
reviewed the X-rays of all those who had fallen ill. They knew they were
facing something very serious and highly unusual.
"All the chest X-rays were abnormal and... were similar to
Johnny Chen. We had a panic attack. We were all thinking that they were
are all going to die," says Cattin.
"One by one, we saw the X-rays and there was a big silence
because we could not talk… We didn't know what was going on. It was
very, very scary."
The virus had a highly unusual pattern of transmission. Its
peak of infectivity occurred late in the course of the disease when its
victims were at their most unwell and usually in hospital care.
Because of this, the worst cases clustered in a few hospital
wards and intensive care units in a handful of major cities. And within
these, the virus spread like wildfire.
When Johnny Chen and some of the first medical staff to care
for him all died, they began to understand what they were facing and the
risk it posed to the world outside.
The 2003 Sars outbreak
|
|
Selected countries
|
Deaths
|
Cases
|
Source: World Health Organization. Cases 1 Nov 2002-31 July 2003
|
China
|
349
|
5,327
|
Hong Kong
|
299
|
1,755
|
Canada
|
43
|
251
|
Taiwan
|
37
|
346
|
Singapore
|
33
|
238
|
Vietnam
|
5
|
63
|
Malaysia
|
2
|
5
|
Philippines
|
2
|
14
|
Thailand
|
2
|
9
|
France
|
1
|
7
|
South Africa
|
1
|
1
|
Total all countries
|
774
|
8,096
|
Full in this knowledge, they took the incredible step of
locking themselves in, quarantining themselves away from the city to
protect it and their country.
"I've never met such amazing doctors and nurses as I did in
North Vietnam," says Cattin. "I lost five colleagues, they were friends.
We're the survivors of this outbreak."
Another survivor is Dr Le Thi Quyen Mai, head of virology at the National Institute of Hygiene and Epidemiology in Hanoi.
"I am very, very lucky," she says. As news of the deadly
virus spread through her institute, most of her colleagues fled, fearing
for their lives. She stayed, despite having a three-year-old daughter
at home.
Why? "Just a duty," she says simply.
In those early days, when events threatened to spiral out of
control, perhaps their most important single asset in the fight against
this outbreak was Carlo Urbani, an Italian expert on infectious diseases
who was working for the World Health Organization (WHO) in Hanoi.
Continue reading the main story
Lock-down in Hanoi
As the news spread of the outbreak at the French hospital in Hanoi, there was uniform panic among the city's residents.
No-one would so much as approach the medical facility. The
street opposite was empty - its shopkeepers pulled their shutters down
and stayed closed. The catering firm that supplied the hospital refused
to deliver.
In the end the French hospital had to get food and drink from
a local hotel - and even then only on the strict condition that they
didn't tell anyone else about the arrangement.
The nurses who remained during the Sars outbreak described
the hospital as having become like a "desert island" - suddenly isolated
and alone in the centre of an otherwise thronging city.
Urbani felt he could not stay in the office as a paper-pushing bureaucrat. As a doctor, he had to help.
It was Urbani who took samples from the patients for analysis
- at great personal risk - and who first alerted the world to the
crisis.
After working tirelessly in the French hospital for several
weeks, he was urged to take a break. And it was then that he discovered
he too had contracted Sars.
"I knew he was getting sicker and sicker," says his eldest son Tommaso Urbani, who was 15 at the time.
"But I hoped from deep down in my heart that he could make it
because he was my father. And I saw him as a strong person, a strong
doctor and thought he was invincible or something like that. So I never
thought that he could die."
But Carlo Urbani did die, two weeks after developing the
illness. Ten years on, Tommaso says he's proud of the sacrifice his
father made.
"I am sure that if he could go back in time, my father would
do exactly the same things. I'm happy for what he did because he saved a
lot of lives."
But although the story of Sars started in Hanoi, it didn't end there.
Johnny Chen, the first patient to arrive in Vietnam suffering
with the virus, was an international businessman who had arrived from
abroad. And so the trail of Sars lead away from Vietnam back to its
original point of explosion - Hong Kong - where Chen had stayed shortly
before.
Continue reading the main story
“Start Quote
I wrote a note to my children. I said, 'I've been exposed, this might kill me'"”
Dr Monica Avendano
"There were two dozen of my
colleagues sitting in the same room, everybody was shaking and running a
high fever, many were coughing," says Prof Joseph Sung who was head of
the Prince of Wales' medical faculty at the time, and was effectively
the man in charge of this unfolding disaster.
"That was the beginning of the nightmare, because from that
day on, every day we saw more and more people developing the same
illness."
Sung divided his team into two groups. One would care for the
other patients in the hospital, and the second team - the "dirty team"
as they called it - would undertake the dangerous job of treating these
patients, and risking infection themselves.
Anyone with young children was given an exemption from the
"dirty team". But those who were single, and those whose children were
grown up, were encouraged to step forward.
Not only did volunteers step forward - they kept on coming during the weeks that followed.
"I needed a continuous supply of manpower to go in. And I was
very touched by the fact that after we exhausted everybody in the
medical department, surgeons, orthopaedics people, gynaecologists, even
ophthalmologists came to help us."
Sung himself ended up spending three months inside the hospital.
In Toronto, half a world away from the East Asian locations
where Sars first arose, the virus took them completely by surprise.
At the Scarborough Grace hospital, a single patient, arriving
unwell with what initially looked like a severe pneumonia, went on to
infect dozens of staff.
Continue reading the main story
“Start Quote
I had Sars - it's left a lasting impact on me and my life. It's still there for me”
Bruce England
Paramedic
Many were transferred to an old tuberculosis hospital on the outskirts of Toronto for quarantine and treatment.
And as in Hanoi and Hong Kong, there were those who chose to
flee and those who turned up for work one day and stayed - without
returning home - for weeks.
"I wrote a note to my children," says Monica Avendano, a
physician and specialist in respiratory diseases at Toronto's West Park
Healthcare Centre, who was one of those who decided to stay.
"I said: 'I've been exposed, I might get infected, this might
kill me and if it does, don't cry too much. I did it because I'm a
physician and I'm a doctor and my duty is to look after sick people.'"
Dr Avendano did survive, but the experience of Sars in Toronto was nothing if not terrifying for those involved.
 Monica Avendano and a colleague at the height of the crisis in Toronto
Monica Avendano and a colleague at the height of the crisis in Toronto
Bruce England was a paramedic on duty in Toronto during the
early days of the Sars outbreak and, having attended a patient with a
chest infection, found himself falling ill.
For him, and many others affected by the Sars outbreak in
Toronto, the effects of that experience are still being felt today. Ten
years on Bruce still experiences weakness and difficulty with his
breathing.
"I had Sars. It's left a lasting impact on me and my life. So did I survive it? Maybe not, it's still there for me," he says.
By the summer of 2003 the chain of human-to-human
transmission had been broken. Doctors had come to understand when the
most contagious times were for anyone infected and what precautions to
take to avoid passing it on.
But what happened in Hong Kong, Vietnam and Toronto could so
easily have happened in London, New York or any destination reachable by
plane.
The vectors of this virus were not rats on ships but aircraft
travelling at hundreds of miles an hour across the globe. The reason
that this is an important story to tell and to continue to retell is
because of how narrowly disaster was averted.
And I now think that the margins were much narrower than we ever realised.





























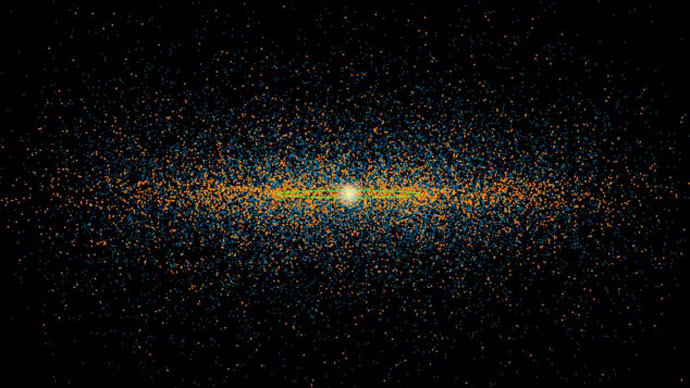
 This graphic shows the orbits of 1,400 Potentially Hazardous Asteroids (PHAs). (Photo by NASA)
This graphic shows the orbits of 1,400 Potentially Hazardous Asteroids (PHAs). (Photo by NASA)

 Wikileaks founder Julian Assange.(Reuters / Suzanne Plunkett)
Wikileaks founder Julian Assange.(Reuters / Suzanne Plunkett)


